
Arthritis is a joint disease accompanied by damage to cartilage tissue. Synonyms for arthrosis are gonorrhea, deforming osteoarthritis, osteoarthritis - all these terms mean the development of degenerative processes in the cartilage that covers the ends of the bones of the body. Osteoarthritis.
Despite the fact that the damage affects only the cartilage structure, all joint components are affected - the joint capsule, synovial membrane, subchondral bone, as well as the ligaments and muscles surrounding the joint. Arthritis can affect one joint or many joints.
The most common localized forms of the disease have their own names: hip arthritis is called coxarthrosis, knee arthritis is called coxarthrosis.
Classification and reasons
Knee arthritis can be primary or secondary. The first group includes pathologies whose cause is unknown, that is, they are idiopathic. Secondary arthritis occurs after trauma, from birth defects, and from systemic diseases.
The following are the causes of knee osteoarthritis:
- autoimmune diseases – rheumatoid arthritis, lupus erythematosus, scleroderma, etc. v. ;
- arthritis caused by specific infections (syphilis, gonorrhea, encephalitis);
- hereditary diseases of the musculoskeletal system and joints, type 2 collagen mutations.
There are also a number of factors that negatively affect the joints and can cause pathological changes in them:
- old age, overweight, osteoporosis;
- Hormonal changes, including reduced estrogen synthesis in postmenopausal women;
- metabolic diseases;
- lack of trace elements and vitamins in the diet;
- Congenital and acquired bone defects;
- hypothermia and intoxication with toxic compounds;
- Continuous joint injuries during sports or hard work;
- operations on the knee joint - for example, to remove cartilage.
Symptoms and stages
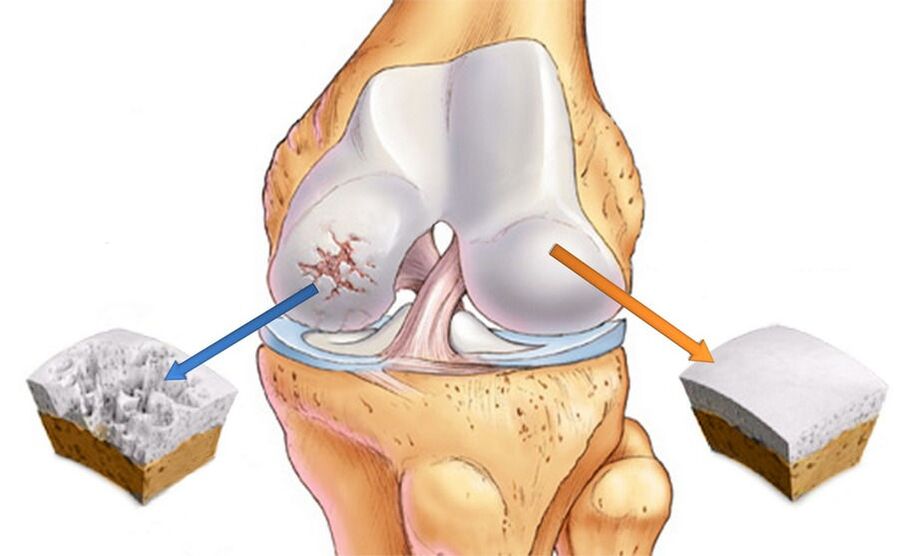
Knee joint deformity is characterized by intracellular changes at the morphological, molecular, biochemical and biomechanical levels. The consequence of the pathological process is that the articular cartilage softens, becomes fibrotic and reduces the thickness of the articular cartilage. In addition, the surfaces of the bones that form joints become denser, and bone spurs - osteophytes - appear on them.
DOA of the knee joint develops in 3 stages and in the early stages may only present with mild pain and discomfort after prolonged physical activity. Sometimes one of the characteristic symptoms of arthritis appears - morning stiffness. At this time, changes occur in the synovial membrane and the composition of the fluid in the joint.
As a result, cartilage tissue does not receive enough nutrients and its ability to withstand pressure begins to decline. Therefore, when exercising intensely and walking for a long time, pain will appear.
In the second stage of arthropathy, the destruction of cartilage tissue progresses and part of the increased load is taken up by the articular surfaces of the bones. Because there is not enough area for support, the edges of the bones will increase due to osteoporosis. The pain no longer goes away when resting like before and makes me uncomfortable even at night.
The time of morning stiffness also increases, the legs have to be "exercised" for a long time before they can walk normally. In addition, when bending the limb, you can hear cracking and clicking sounds, accompanied by a sharp pain. It is not always possible to completely bend the leg, it seems to be stuck, and further attempts will end in severe pain and crunching.

Due to the appearance of pain when moving, a person tends to move less, which negatively affects the muscles around the joints. Changes in the size of the bone ends lead to displacement of the limb axis and development of deformities. The joint capsule becomes stiffer as the volume of fluid in it decreases. When bone spurs compress surrounding soft tissues, synovitis and chronic inflammation occur.
When entering stage 3, the signs of knee osteoarthritis become very severe - the pain does not improve even at night, mobility almost stops, the legs look crooked and cannot be bent. The third degree of osteoarthritis is characterized by an X- or O-shaped deformity, making movement extremely difficult. A progressive disfiguring form of gonorrhea that can only be treated with surgery.
Diagnose
Diagnosing osteoarthritis of the knee is not particularly difficult; your doctor can diagnose gonorrhea based on the symptoms present and characteristic visual signs. To confirm the diagnosis, an X-ray is performed. The images will show narrowing of the space between joints, bone growth, and subchondral bone sclerosis.
X-rays are used to determine the cause of the disease. Bone deformities are especially evident in posttraumatic arthritis. If cartilage degeneration is due to arthritis, defects along the bone margins as well as periarticular osteoporosis and atrophy of bone structures will be detected. With various congenital malformations, deformation of the axis of one of the bones is observed, which leads to improper distribution of the load and the occurrence of secondary osteoporosis.
Treatment
Treatment of knee gonorrhea has 3 main goals - restoring cartilage tissue, improving joint mobility and slowing the progression of the disease. Great importance is attached to the elimination or weakening of symptoms - reducing the intensity of pain and inflammation. To address these problems, medications, physical therapy, and exercise therapy are used. To achieve maximum therapeutic effect, it is necessary to do physical activity in accordance with the dosage and compliance with the orthopedic regimen.
Drug treatment for knee arthritis includes pain relievers and anti-inflammatory drugs, as well as chondroprotective drugs that promote cartilage tissue regeneration. The medicine can be prescribed as injections, tablets, ointments and gels.
If grade one knee arthritis is diagnosed, physical therapy, physiotherapy and massage methods will be used in treatment. The early stages of the disease are much easier to treat and you can expect a full recovery. An important condition is weight loss to reduce the load on painful joints.
Treatment of stage two knee arthritis necessarily includes exercise therapy, wearing orthotics, and following a diet. To relieve pain, non-steroidal anti-inflammatory drugs, chondroprotectors and injections of hyaluronic acid into the joint are prescribed.
Acute arthritis is characterized by severe pain for which conventional NSAIDs are inadequate. In this case, strong painkillers and glucocorticosteroid injections into the joint cavity are used.
If conservative methods are ineffective, surgery will be performed, which can be corrective or radical (joint replacement with a prosthesis).
Knee deformity in the third stage is characterized by the complete absence of the space between the joints, which is replaced by bone structures. This condition requires surgical intervention because other methods are ineffective in this case.
NSAIDs and corticosteroids
To save the patient from physical and mental suffering, therapy for acute arthritis begins with pain relief. Medications that belong to the NSAID group and can be used in pill form or applied topically have been shown to be effective.
The pain relief effect does not always occur immediately, but after two or three days it will reach its peak and the pain will disappear. Treatment with NSAIDs is limited to two weeks, as longer use increases the risk of side effects. Particular caution is required for people with gastrointestinal problems, as well as people with high blood pressure.
If there are no results, hormonal drugs are prescribed to reduce inflammation. In case of left gonorrhea, the drug is injected into the left knee, in the right - on the right.
Hormonal injections can be given every 10 days, not more often. The indication for such treatment is a large accumulation of fluid in the joints due to inflammation. When symptoms subside, they switch to pills.
Chondroprotectors and hyaluronic acid
Chondroprotectors act in three directions - they restore damaged cartilage tissues, relieve pain and eliminate inflammatory reactions. Taking chondroprotectors helps normalize the composition and properties of joint fluid, nourishes cartilage and protects pain receptors from irritation.
The result is destruction of the cartilage structure and, as a result, the progression of the disease slows down. After a period of taking the drug, the shock absorption and lubrication functions of the joints are restored.
In the early stages of the disease, chondroprotectors can be used in the form of ointments or gels. However, intra-articular injections are the most effective. Modern methods of treating arthrosis include the use of combined agents that contain not only cartilage-protecting substances, but also anti-inflammatory components and vitamins.
Hyaluronic acid is the main component of synovial fluid, responsible for its viscosity and consistency. In fact, this is a biological lubricant that provides cartilage with elasticity, elasticity and strength.
With the development of joint pathologies, the amount of hyaluronic acid can decrease 2-4 times, which necessarily leads to excessive friction of the bones. With injection of hyaluron into the joint, the function of the knee is normalized and the patient can move normally.

Surgery
Surgery is a radical method to restore partial or full function of the joint. The level of intervention may vary and depends on the stage of arthritis. The most gentle operation is arthroscopy - the recovery period after the procedure is the least painful for the patient.
Important:Arthroscopy can be performed not only to treat but also to diagnose joint pathology. This procedure allows you to determine damage that is inaccessible to other studies.
The goal of arthroscopy is to prolong the life of the joint by removing dead and damaged tissue from the joint cavity. As a result, pain disappears, resistance to stress increases, and motor activity returns.
In case of significant deformation, osteotomy is indicated - creating an artificial fracture in a specific area. Knee osteotomy literally means "cutting the bone" - during surgery, the surgeon removes a wedge-shaped segment of the femur or tibia, then grafts the bones in the most physiological position. If necessary, the resulting space will be filled with bone graft. During the healing period, the structure is fixed with special clamps.
Arthroscopic replacement is an alternative to outdated joint treatment procedures, the essence of which is to replace part or all of a diseased joint with a prosthesis. As a result, knee function is completely restored in more than 90% of cases, significantly improving the patient's quality of life.

Physical therapy
Physiotherapy procedures play an important role in the treatment of joint diseases, due to their beneficial effects on damaged joints. A course of physiotherapy accelerates the regeneration process, eliminating pain and muscle spasms. Additionally, certain procedures allow delivery of the drug through the skin, thereby reducing the oral dosage.
For damaged joints, the following techniques should be applied:
- magnetic therapy;
- mid-wave ultraviolet (WUV);
- infrared laser;
- UHF;
- supersonic;
- sinusoidal and diademic modulated currents (amplification therapy);
- Darsonval.
Effective procedures for treating arthritis are also therapeutic baths - radon, hydrogen sulfide, bischofite, minerals and sage. They have anti-inflammatory, pain-relieving and joint-restoring effects.
Final
If you suspect you have knee arthritis, you should consult an orthopedist or traumatologist to diagnose and treat these conditions. In order not to aggravate the disease, it is necessary to avoid excessive physical activity on the legs and eliminate excess weight.
There is no special diet for arthritis, but you should avoid strong meat and fish broths, fatty meats and smoked meats, and reduce your consumption of table salt. The diet should consist mainly of foods rich in vitamins, minerals and vegetable oils. In addition, once a week it is recommended to arrange a fasting day - kefir, cheese or fruits and vegetables.
To strengthen the muscles of the lower limbs and increase blood flow, it is necessary to regularly perform therapeutic exercises individually selected by the physiotherapy instructor.
So, medication, physical procedures, a balanced diet and exercise are things that will definitely help patients with joint diseases. And to avoid needing surgery due to injury, you should seek medical help as soon as possible. Be healthy!



























